Altitude sickness in babies can present itself as the baby seeming visibly uncomfortable and beginning to throw up when traveling to the mountains or higher altitudes. It might be stressful for the parents to see their baby in distress or discomfort. Read this post to know more about the causes, types, signs, diagnosis, treatment, and prevention of altitude sickness in babies.
What Causes Altitude Sickness In Babies?
Altitude sickness is an umbrella term for a group of symptoms that might occur when you travel to a place at a high altitude. It is also known as ‘mountain sickness.’
The air in the atmosphere exerts pressure on earth. It is known as barometric pressure. As we go higher in altitude, this pressure begins to drop. Along with the pressure, the oxygen level in the surrounding atmosphere also falls.
Multiple changes in the atmosphere affect the body, thus causing altitude sickness and making the baby feel uncomfortable.
Is It Safe For A Baby To Visit High-altitude Areas?
It is safe to travel to high-altitude places once the baby is more than six weeks old (1). You may follow some precautions during the trip.
- Seek your pediatrician’s consent before traveling to places of high altitude. The doctor’s approval is vital if your baby was premature, unwell recently or has a medical condition. They may prescribe any emergency medications for altitude sickness.
- If your baby has a frequent need for supplemental oxygen, that is, requires oxygen inhalation through a machine or cylinder, then it is advised against visiting a place at high altitude.
- Babies with pulmonary hypertension, a form of high pressure in the lungs causing low oxygen levels in the blood, should be avoided from being taken to such places.
Keep your baby hydrated with breast milk and water, once you have observed all the precautions and reached a high altitude region. Feed your baby small but multiple meals a day if they are on solids. Babies younger than six months should be given only breast milk.
How To Take Care Of A Baby Having Altitude Sickness?
You can observe the following simple non-pharmacological methods to help the baby with altitude sickness feel better.
- Hydrate your baby through breast milk or formula. If your baby is older than six months, then you can provide them with frequent sips of water.
- Feed your baby small yet frequent meals that are high in carbohydrates. It is noted that craving for carbohydrates tends to increase at high altitudes (2). Carbohydrates may help provide sufficient energy to the body to overcome altitude sickness
- Regions at a high altitude are often cold. Dress your baby in insulated clothing. Staying warm may help the baby feel better.
A baby can be prone to altitude sickness even when they are healthy. It is thus essential to know the variations of altitude sickness.
Types Of Altitude Sickness
Altitude sickness occurs in various levels of severity. It is broadly classified into three different syndromes.
1. Acute mountain sickness (AMS)
This is the most common form of altitude sickness but is less severe (3). Healthy babies may also have AMS.
2. High altitude pulmonary edema (HAPE)
HAPE occurs when fluid accumulates in the tissues and air spaces within the lungs (4). This leads to the impaired exchange of gasses and may cause respiratory failure. HAPE has the symptoms of AMS (listed later) accompanied by breathlessness, coughing, and weakness. Oxygen support or descent might be life-saving.
HAPE is significantly less common than AMS. Babies with the following conditions tend to be more susceptible to HAPE (1) (5).
- Recent viral infections
- Recent upper respiratory tract infections
- Pulmonary hypertension (high blood pressure)
- Problems with pulmonary artery and pulmonary vein
- Atrial and ventricular defects (heart defects)
- Obstructive sleep apneaiXA sleep disorder in which there are recurrent episodes of breathing pauses.
- Babies with Down’s syndromeiXA chromosomal disorder caused by the presence of an extra copy of chromosome 21, resulting in intellectual impairment and short stature. might be more prone to HAPE.
3. High altitude cerebral edema (HACE)
High altitude cerebral edema is considered the most severe form of altitude sickness but is also the rarest (6). The condition occurs when there is an influx of fluid and swelling of the brain due to low oxygen in ambient air (7). Along with all the symptoms of AMS, HACE has profound lethargy, drowsiness, dizziness, confusion, and poor muscle control.
HAPE and HACE can be fatal, and usually, a prompt descent to a low altitude is suggested. Since AMS can aggravate HAPE or HACE, it is essential to know the symptoms of altitude sickness in babies.
What Are The Signs Of Altitude Sickness In Babies?
If you just traveled with your baby to a high altitude location, then be alert to the following general indicators of altitude sickness.
- Fussiness
- Food refusal
- Crying
- Irritability
- Clinginess
- Lethargic
Some symptoms, such as severe crying and irritability, may also happen due to tiredness from the trip. So let your baby rest well. If the symptoms persist even after resting, then it could be acute mountain sickness.
There are a few severe symptoms of altitude sickness that could point towards HAPE and HACE.
- Breathlessness
- Cyanosis, a bluish discoloration of the skin
- Confusion
- AtaxiaiXA term that refers to a lack of muscle control, coordination, and body balance., poor muscle control and inability to move
- Coughing
- Repeated vomiting
When Should You Call The Doctor?
See a doctor during the following situations:
- The baby shows severe symptoms of altitude sickness
- General symptoms of AMS persist for more than three days.
- There is labored breathing with constant shortness of breath.
- Repeated vomiting and dehydration
- Refusal to eat or drink
These problems require prompt medical attention.
The symptoms of altitude sickness could overlap with other conditions. Also, a baby cannot verbally express discomfort. Therefore, a score-based diagnostic tool could be used to determine if the baby has altitude sickness.
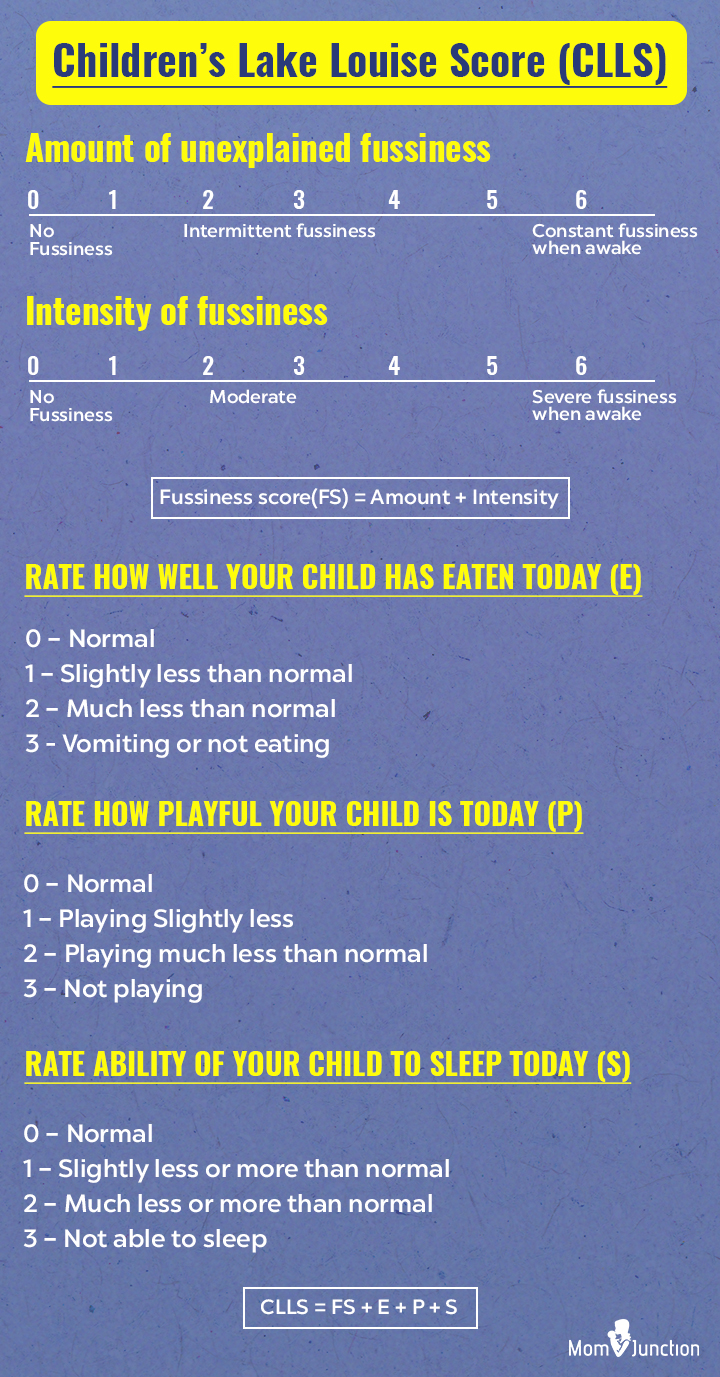
How To Diagnose The Severity Of AMS In Your Baby?
The severity of altitude sickness may be determined through the use of Children’s Lake Louise Score (CLLS) for the diagnosis of acute mountain sickness (AMS) in preverbal children (8).
The process begins by rating the amount and intensity of baby’s fussiness measured on the following scales.
Meeting all of the following score conditions determines the presence of acute mountain sickness:
- Fussiness score (FS) should be greater than or equal to 4
- Eating, playfulness, and sleep score (E+P+S) should be greater than or equal to 3
- The total Children’s Lake Louise Score (CLLS) should be greater than or equal to 7
CLLS is useful in providing an approximate idea to the parents about the severity of altitude sickness in their baby. It is best to consult a doctor if you have any concerns or when the baby displays severe symptoms of altitude sickness.
How Is Altitude Sickness In Babies Treated?
The doctor may suggest the following treatment methods to help the baby feel better.
- Medications: If the baby is feeling excessively fussy and restless, then the doctor may prescribe ibuprofen or acetaminophen. Do not self-medicate even with over-the-counter medicines.
- Electrolyte supplement: If the baby is dehydrated due to vomiting and is feeling dizzy, then the doctor may suggest an electrolyte solution such as an oral rehydration salt (ORS). It may help subdue nausea and constant discomfort caused by altitude sickness.
- Descent to low altitude: If the condition of the baby does not seem to improve, then the last resort will be moving to a place with a low altitude.
Do not give acetazolamide, nifedipine, and dexamethasone to the baby. These medicines are conventionally administered to teens and adults for altitude sickness. But their effect on infants is not well known, and it may cause side effects. Consult your doctor before giving any medicine to the baby.
How To Prevent Altitude Sickness In Babies?
A few simple steps can help you avoid altitude sickness in babies (9).
- Avoid flying directly to an altitude above 2,750 meters (9,000 feet). The baby’s body will have no time for acclimatization.
- Ascend 1,000 feet (305 meters) at a time. Spend a day at that altitude before moving any further. It will help your baby’s body to get used to the increasing altitude gradually.
- Let your baby rest. Make sure they are not fussy, cranky, and tired before your trip to the high-altitude location.
- Hydrate the baby as you reach a high-altitude location.
Does High Altitude Make A Baby Have Ear Infections?
There is no direct link between living at high altitudes and ear infections. Changes in altitude may increase the risk of infection (10). However, the risk might be due to related changes in climate since places at a higher elevation tend to be colder. If your baby has enough time to acclimatize to the altitude and weather, then they may be less prone to ear infections. In addition, exposure to a hypobaric environment like that at a high altitude can lead to oxygen deprivation and potentially increase the risks for conditions such as respiratory distress, headaches, and fatigue (7).