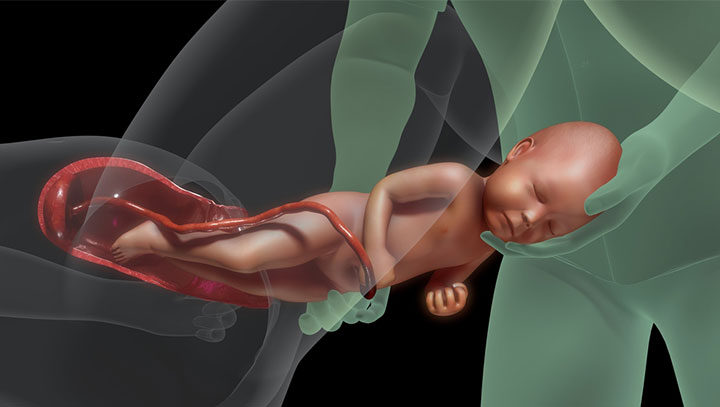
Congenital diaphragmatic hernia in babies or CDH in babies occurs when the diaphragm fails to close during fetal life. The diaphragm is a muscular wall separating the chest and abdominal cavity. If there is an opening, the abdominal organs may herniate or protrude to the chest cavity and affect lung growth.
Babies with CDH may develop pulmonary hypoplasia (resulting in a smaller lung) and pulmonary hypertension (high blood pressure in the lung arteries). Prompt medical care soon after birth may reduce the complications of CDH in babies. However, such babies have an increased risk for morbidity and mortality.
Read on to know about the causes, symptoms, types, complications, diagnosis, and treatment of CDH in babies.
Causes Of CDH In Babies
The cause of CDH is unknown in many babies. It is believed to be multifactorial. Some research suggests that genetic factors may cause CDH, especially when it occurs with other birth defects, such as congenital heart defects. However, CDH may also be an isolated anomaly in some babies with no other genetic defects (1).
Source: Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities
Types Of CDH
CDH can be of two types (2).
- Posterolateral Bochdalekhernia is the common type (70-75%), occurring due to a hole in the diaphragm’s back. Majority occur on the left side.
- Anterior (Morgagni) hernia (23-28%) occurs due to a hole in the front of the diaphragm. This type of hernia has less impact on lung growth.
- Central (2-7%)
Signs And Symptoms Of CDH
The following signs and symptoms are seen before birth on the prenatal ultrasound.
- Fluid in the chest
- Displaced heart
- Herniation of liver, intestines, and stomach to the chest cavity
Bochdalek hernia usually causes more severe symptoms (3).
- Fast breathing (tachypnea) or breathing difficulties
- Increased heart rate (tachycardia)
- Bluish skin or cyanosis
- Barrel-shaped chest or chest with abnormal shape, such as one side may look more extensive than the other
- Caved in or scaphoid appearance of the abdomen
- Symptoms of respiratory distress such as grunting respiration and chest retractions
- Other congenital anomalies including cardiac, vertebral, ear etc.
Some babies with CDH may require aggressive resuscitation due to underdeveloped lungs and circulatory insufficiency. Respiratory distress and cyanosis immediately or a few minutes or hours after birth can be commonly seen in babies with CDH.
Prognosis
All of the following factors are associated with increased risk of mortality and morbidity:
- Presence of associated anomalies, especially those of heart
- Extensive underdevelopment of lungs or lung hypoplasia
- Liver entering chest cavity
Complications Of CDH
After the immediate neonatal period CDH could be associated with the following complications (2).
- Hernia recurrence
- Failure to thrive
- Inability to feed, requiring feeding through tubes
- Chronic lung diseases requiring oxygen therapy such as oxygen supplementation and medications for a long time
- Pulmonary hypertension
- Repeated lung infections
- Developmental delay
- Gastroesophageal reflux (abnormal positioning of the stomach)
- Hearing impairment
- Chest wall deformities such as scoliosis and pectusiXA condition where breastbones grow inwards, causing a mild or severe depression of the chest wall
Complications may vary based on the severity of the CDH. Early interventions are required to minimize the effect of these complications and reduce the risks of any long-term complications.
Diagnosis Of CDH
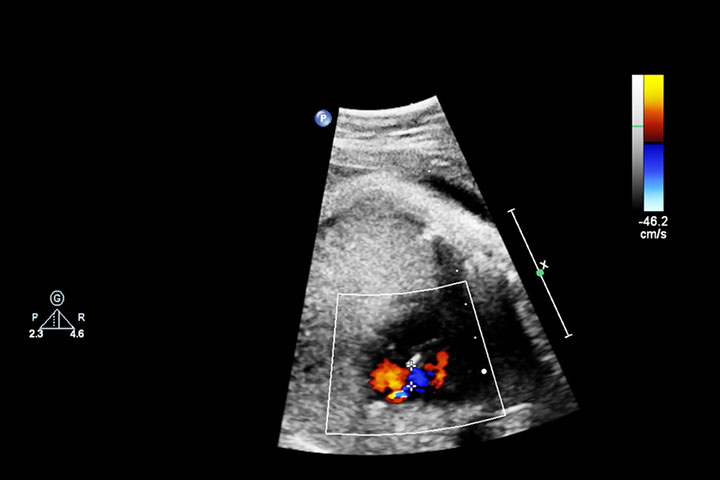
CDH is diagnosed during prenatal ultrasound since the abdominal organs, such as the stomach, liver, and intestine, may be seen in the chest cavity. These abdominal organs may push the heart to one side.
The following imaging techniques are often ordered to confirm the prenatal diagnosis of CDH (1).
- High-resolution fetal ultrasound to evaluate the fetal anatomy and CDH
- Fetal echocardiogramiXUse of sound waves to examine baby’s heart issues before birth to assess structure and functions of the fetal heart
- Ultrafast fetal MRI also helps to visualize the anatomy and CDH
These tests identify the affected part of the diaphragm and the displaced organs. CDH may affect the left, right, or both sides of the diaphragm. The impact of CDH on the lungs is also noted to estimate the consequences after birth.
Arundhati Sharma, a mother, recalls her experience when an ultrasound at 24 weeks of gestation showed a possibility of the fetus having CDH. She says, “The radiologist told me the baby is suffering from CDH (Congenital Diaphragmatic Hernia), she further explained that the intestine is pushing our baby’s heart over the right side of its chest, which may hinder his lung growth. After a few minutes, she called in a doctor to study the ultrasound, who then ordered a series of additional tests.” A fetal MRI confirmed the doctor’s suspicion (i).
Treatment Of CDH
Treatment options may vary depending on the severity of CDH and the age of the baby. The treatment can be prenatal or postnatal (4).
1. Management during pregnancy
You may receive a referral to a maternal-fetal medicine specialist and a pediatric surgeon if the prenatal ultrasound shows signs of CDH. The obstetric team managing CDH pregnancies may observe the CDH pregnancies every four weeks until the last trimester and every week after that.
Lung dimensions and amniotic fluid volume measurements on ultrasound are done at frequent intervals during the prenatal period. If the CDH is severe, fetal surgery is considered. Fetoscopic endoluminal tracheal occlusion (FETO) is a fetal surgery for CDH. Treatment before birth could help the baby’s lungs grow correctly and avoid life-threatening complications.
2. Delivery of babies with CDH
If the CDH is diagnosed during the prenatal period, delivery is planned in a multispecialty hospital since the baby may require medical care immediately after birth. Most babies with CDH are delivered vaginally at term if there are no obstetric issues necessitating cesarean section.
Many newborns with CDH are transferred to neonatal intensive care units for postnatal care. Breathing tubes and a ventilator (breathing machine) are connected to babies with respiratory distress. A nasogastric or orogastric tubeiXSoft tubes inserted through the nose or the mouth into the stomach to provide food or medication is also inserted to keep the stomach decompressed since this may help the lungs expand. Many babies require extensive NICU care for many days.
3. Surgical repair of CDH
Surgical repair of CDH is done through an incision below the rib cage. The time and type of surgery may vary based on the severity and health status of the baby. Medications and inhalation therapies are also given before surgery to enhance lung function. It should be understood that though surgery is a part of long term management it seldom produces acute relief of symptoms.
A Gore-Tex patch or a muscle flap is used to close the diaphragmatic opening, depending on its size. Regular follow-up is done for a few years to observe lung growth in babies.
4. NICU stay for babies with CDH
Babies are kept in NICU since these facilities are immediately available for stabilization. Nitric oxide, high-frequency oscillatory ventilation (HFOV), and ECMO (heart-lung machine) may be required for CDH management.
HFOV can deliver air and pressure against pulmonary hypertension as compared to standard ventilators. ECMO machines take over the functions of the heart and lungs in the body. This provides rest to the lungs and avoids complications due to inadequate lung and heart functions in babies.
The length of hospital stay and outcomes may vary based on the severity of CDH. These babies require follow-up care.
Sharing how the baby’s condition was managed in the hospital after her son was born, Sharma says, “The very next day, his CDH surgery was performed. I was allowed to see him immediately after his surgery… He was kept in an isolated ward so that he didn’t catch any infection, which could result in slow recovery and septic on the stitches. He spent the next two weeks in the NICU.” The child survived the surgery and recovered well.
Congenital Diaphragmatic Hernia in Babies may sometimes lead to complications. It is diagnosed before birth through ultrasound and other imaging modalities. The doctor may carry out this treatment before or after birth based on the severity of the condition and other morbidities. Although CDH in babies is concerning, early diagnosis can help with the timely treatment of the baby. With prompt treatment and necessary preventive measures, there is hope for a positive outcome with a healthy functioning heart and lungs.
Key Pointers
- Faulty closure of the diaphragm in a fetus causes congenital diaphragmatic hernia or CDH in babies.
- Posterolateral Bochdalek hernia and anterior (Morgagni) hernia are the two types of CDH.
- Neonates with CDH may have complications such as chronic lung diseases, increased lung pressure, or developmental delays.
- Fetal surgery may be considered if severe CDH is detected in ultrasounds.
Congenital Diaphragmatic Hernia is a birth abnormality in which the diaphragm is affected, causing abdominal organs to be displaced into the chest cavity. Learn more in this video!